Mohamed Sorror and Mary-Elizabeth Percival contributed equally to this project.
Introduction:
There has been inconsistent evidence supporting the association between obesity and outcomes in patients with newly diagnosed acute myeloid leukemia (AML). Prior studies have studied obesity as defined by body mass index (BMI) ≥ 30. However, this general definition of obesity can be further subdivided into class I obesity (BMI 30 to <35), class II obesity (BMI 35 to <40) and class 3 obesity (BMI ≥40). Given the high prevalence of obesity in the United States (41.9%; with class III obesity 9.2%), distinctions in degree of obesity may be associated with outcomes for patients with AML (Stierman et al, 2021). We were interested in studying outcomes in patients with AML stratified by class I, class II and class III obesity after induction chemotherapy and allogeneic hematopoietic cell transplant (HCT). Identification of at-risk patient populations could aid in design of future interventions.
Methods:
We retrospectively reviewed a group of 738 previously untreated subjects with AML randomized to daunorubicin and cytarabine (DA), idarubicin and cytarabine (IA), and IA with vorinostat as part of clinical trial SWOG 1203, conducted by the SWOG Cancer Research Network between 2012 and 2015. Subjects with adverse risk cytogenetics were recommended to receive HCT in their first complete remission (CR1); subjects with intermediate risk cytogenetics were selected for HCT in CR1 per local institutional standards. Nine patients who did not receive protocol therapy or had missing BMI were excluded (final cohort 729 patients). Early death was defined as death within 56 days of induction chemotherapy. Multivariable time-dependent Cox regression model and Fisher's exact test were used for analysis of overall survival (OS). HCT in first complete remission (CR1) was included as a time-dependent covariate.
Results:
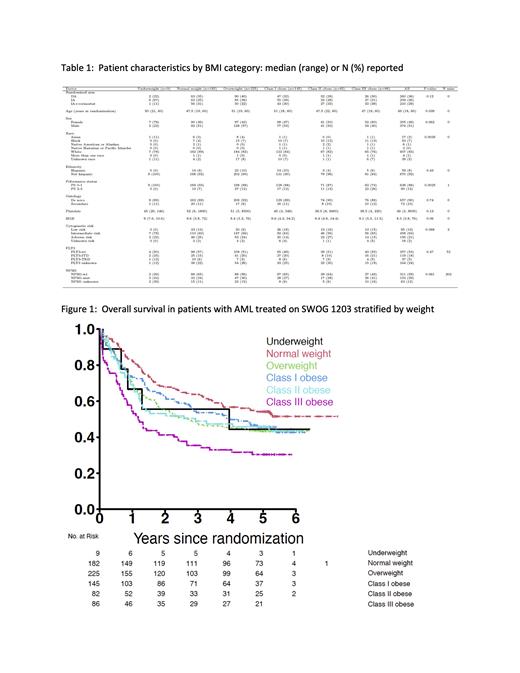
The median age was 49 years (range, 18 to 60), 51% were male, 90% had de novo disease, and 88% had a performance status (PS) of 0-1 (Table 1). Among these patients, 1% (n=9) were underweight, 25% (n=182) were normal weight, 31% (n=225) were overweight, 20% (n=145) had class I obesity, 11% (n= 82) had class II obesity and 12% (n= 86) had class III obesity. There was no difference in the rate of achieving composite CR (CR with or without count recovery) between different weight categories (p=0.17). There was no clear trend in early death rate by weight (underweight: 11%; normal weight: 4%; overweight: 6%;class I obesity: 7%; class II obesity: 4%; class III obesity: 17%), though class III obesity had a significantly higher early death rate as compared to all the other groups combined (p=0.004). In multivariable Cox regression analyses, class III obesity was significantly associated with worse OS when compared to normal weight (hazard ratio (HR) 2.56, 95% confidence interval (CI) 1.68-3.90; p<0.001); though not statistically significant, we identified a trend towards worse OS for patients with class I (HR 1.40, 95% CI 0.95-2.06; p=0.09) and class II obesity (HR 1.48, 95% CI 0.95-2.31; p=0.09) (Figure 1). Other co-variates with a significant association with OS included age (HR 1.03, 95% CI 1.01-1.04; p<0.001), intermediate cytogenetic risk (HR 2.45, 95% CI 1.33-4.51; p=0.004), and adverse cytogenetic risk (HR 5.86, CI 3.10-11.06; p<0.001). HCT during CR1 was not found to be significantly associated with OS (HR 0.88, CI 0.67-1.15; p=0.3). No significant difference was identified in time to HCT based on BMI category. In patients who underwent HCT during CR1, class III obesity (HR 2.32, 95% CI 1.22-4.43; p=0.01) and older age (HR 1.02, 95% CI 1.00-1.04; p=0.01) were significantly associated with worse OS; in contrast no significant association was identified between OS and class I obesity (HR 1.30, 95% CI 0.77-2.20;p=0.32), while a higher HR and a trend existed for class II obesity (HR 1.76, 95% CI 0.97-3.17; p=0.06).
Conclusions:
Our retrospective analysis suggests that among newly diagnosed younger patients with AML, those with class III obesity are at increased risk of early death and shorter overall survival. Future directions include assessing lean body mass in addition to BMI in patients with newly diagnosed AML, as sarcopenic obesity is known to portend poor outcomes. Identifying this at-risk patient population may help guide future investigation of early weight management interventions in patients with newly diagnosed AML.
Disclosures
Erba:AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Amgen: Research Funding; Ascentage: Research Funding; Sumitomo: Research Funding; Forma: Research Funding; Forty-Seven: Research Funding; Gilead: Research Funding; PTE: Research Funding; ALX Oncology: Research Funding; Trillium: Consultancy; Genentech: Consultancy; BMS: Consultancy, Honoraria, Other: Chair, Myeloid Neoplasms Repository Study; Daiichi Sankyo Inc.: Consultancy, Research Funding; Celgene: Consultancy, Honoraria, Other: Chair, Myeloid Neoplasms Repository Study, Research Funding; Glycomimetics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Astellas: Consultancy; Immunogen: Consultancy, Research Funding; Incyte: Consultancy, Honoraria; Jazz Pharma: Consultancy, Honoraria, Research Funding; Kura Oncology: Consultancy, Research Funding; Macrogenics: Consultancy, Research Funding; Sunesis Pharmaceuticals: Honoraria; Agios: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy; Servier: Consultancy, Honoraria, Research Funding; Syros: Consultancy; Takeda: Consultancy. Garcia-Manero:Genentech: Research Funding; Bristol Myers Squibb: Other: Medical writing support, Research Funding; AbbVie: Research Funding. Pagel:Loxo Oncology at Lilly: Current Employment. Sorror:JAZZ pharmaceuticals: Consultancy; BlueNote and Massachusetts General Hospital: Research Funding. Percival:Abbvie: Research Funding; Ascentage: Research Funding; Astex: Research Funding; Biosight: Research Funding; BMS: Research Funding; Glycomimetics: Research Funding; Pfizer: Research Funding; Telios: Research Funding.